Arthritis - More than Physical Discomfort - Let’s Talk About Social Interaction
Arthritis is one of the most common medical conditions diagnosed in the United States and world-wide. CDC US data notes there are approximately 60 million individuals battling arthropathy with that estimate rapidly growing to an estimated 78 million (26%) US adults aged 18 years or older projected to have doctor-diagnosed arthritis by 2040.
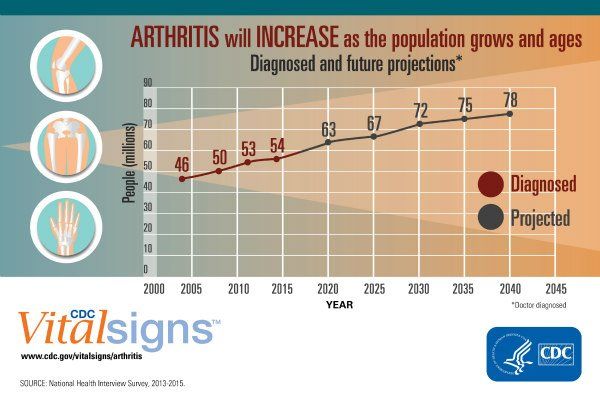
Some reviews state this CDC data is underestimating the future prevalence of arthropathy as individuals generally live longer coupled with rising average population body mass indexes (BMI) – which leads to more shear stress on weight bearing joints like the lumbar spine / hips / knees. Either way we look at this – this is an enormous disease burden that is accelerating in incidence yearly and more than 1 out of every 4 US adults will have diagnosed arthropathy in the near future.
The issue here is that arthropathy simply does not lead to pain/discomfort. There are other tremendous downstream affects of chronic joint pains. This blog post will focus on the mental impacts of arthropathy. There is growing data that individuals with arthritis have a markedly increased risk of social isolation (when adults become lonely) and diagnosed depression.
In a study published in the Journal of the American Geriatrics Society – researchers combed the EPOSA Study and examined the relationship between osteoarthritis and social interactions. This study pool included 2,942 adults between 65-85 years of age living in Germany, Italy, the Netherlands, Spain, Sweden, and the UK which led to 1,967 active participants. Researchers used questionnaires that logged how often and how many times the participants connected socially with friends and family members. They also learned how often the participants volunteered or participated in social activities.
Study results indicated approximately 20 percent of individuals were classified as having social isolation at the baseline (start) of the study with a 13% additional incident diagnosis of social isolation found 12 to 18 months after baseline. The study concluded that OA independently increases the risk of incident social isolation onset. People with hip and/or knee OA particularly are at increased risk of social isolation in a community cohort. The presence of cognitive impairment and worse walking times in both sexes and depression in the females also increased the risk of becoming socially isolated during the follow-up period. Osteoarthritis also remained an independent predictor of worse outcomes in the multivariate analyses, even after adjusting for functional limitations and pain scoring.
Social isolation is not a benign condition and can increase multiple health risks for individuals. Below is a chart highlighting four variables that proved significant in analysis: clinical OA, cognitive impairment, depression, and walking time.
A report based on the United States population from the National Academies of Sciences, Engineering, and Medicine (NASEM) points out approximately 40% of adults over age 45 having limited social interactions overall with nearly one-fourth of adults aged 65 and older considered to be overtly socially isolated (lonely). This report highlighted glaring potential health impacts for those with social isolation including:
- Social isolation significantly increased a person’s risk of premature death from all causes, a risk that may rival those of smoking, obesity, and physical inactivity
- Social isolation was associated with about a 50% percent increased risk of dementia
- Poor social relationships (characterized by social isolation or loneliness) was associated with a 29% increased risk of heart disease and a 32% increased risk of stroke
- Loneliness was associated with higher rates of depression, anxiety, and suicide
- Loneliness among heart failure patients was associated with a nearly 4 times increased risk of death, 68% increased risk of hospitalization, and 57% increased risk of emergency department visits
So we know a few things from these reviews – that arthropathy increases rates of social isolation and that social isolation itself has a plethora of physical and mental health complications that go as far as to increase mortality risks (death). We as physicians/clinicians need to understand and own these facts and regularly discuss and screen for impaired social interactions and overt depression in our patient cohorts. We need to implement active treatment plans to help those in need and potentially improve our overall patient outcomes and quality of life.
If yourself or someone you know is suffering from impaired social interactions or overt social isolation (loneliness). Here are some suggestions to get active again:
- See your Primary Care, Geriatrician, or Mental Health expert to assess social interaction/depression screening and potential therapy options
- Arthropathy management – can focus on anti inflammatory agents (such as Organic Arthritis) or physical therapy to help control root cause symptoms that often times lead to decreased activity, mobility, and social interaction. You can learn more about potential therapy options on our OA Blog
- AARP—Provides helpful information to seniors to help improve quality of life and provides access to Community Connection Tools.
- Area Agencies on Aging (AAA)—A network of over 620 organizations across America that provides information and assistance with programs including nutrition and meal programs (counseling and home-delivered or group meals), caregiver support, and more. The website can help you find your local AAA, which may provide classes in Tai Chi and diabetes self-management.
- Eldercare Locator—A free national service that helps find local resources for seniors such as financial support, caregiving services, and transportation. It includes a brochure that shows how volunteering can help keep you socially connected.
- National Council on Aging—Works with nonprofit organizations, governments, and businesses to provide community programs and services. This is the place to find what senior programs are available to assist with healthy aging and financial security, including the Aging Mastery Program® that is shown to increase social connectedness and healthy eating habits.
- National Institute on Aging (NIA) – Provides materials on social isolation and loneliness for older adults, caregivers, and health care providers. Materials include health information, a print publication available to view or order no-cost paper copies, a health care provider flyer, and social media graphics and posts.
Sending good vibes and wishing everyone the absolute best. Feel free to reach out anytime with any questions. Stay healthy and stay active everyone!











