What is Osteoarthritis?
Dr. J | a board certified Internist and Nephrologist practicing in the DC/Metropolitan area with over 30 years of clinical experience
In a previous blog post we defined the overall category of arthritis and discussed some of the metrics showing the marked public health burden (and rapid growing prevalence) it encompasses. Now let us start breaking down some of the entities under the umbrella of arthritis. By far the most common issue is osteoarthritis.
Risk factors for degenerative joint disease include:
- Age - risk for OA rises as an individual (and the individual’s joints/cartilage/muscles) age
- Joint overuse - repetitive force placed on particular joint
- Joint trauma – fracture or cartilage damage or tear
- Obesity - Extra weight will increase force/stress on joints + fat cells promote inflammation
- Muscle injury/weakness – Joints can have force/stress if muscles do not provide support
- Gender – women typically have a slightly increased chance to develop OA
- Genetics – there is a potential genetic risk association
The most common locations of osteoarthritis are the weight bearing joints of the knees, hips, lower back, lower neck, and small joints of the fingers/toes. This inflammation can manifest clinically as:
- Pain/Ache
- Swelling/Inflammation of joint
- Stiffness / Decreased range of motion (or flexibility)
- Muscle Weakness (typically around the joint)
- Balance/Gait instability/Falls – depending on the joints affected
The Arthritis Foundation notes
that individuals with OA are almost three times more likely to develop cardiovascular disease (CVD) or heart failure than those without OA, studies show. Also, people with osteoarthritis experience as much as 30 percent more falls and have a 20 percent greater risk of facture than those without OA. These links are especially strong when arthritis is in certain joints, such as the knee/back/hip.
It makes sense – pain/weakness especially in our stabilizing joints such as knees/hips/spine will limit mobility and lead to risk factors such as weight gain, cardiovascular disease, diabetes coupled with stability issues. These patients would have difficulty following American Heart Association recommendations
stating that increasing physical activity and becoming more active can help lower your blood pressure and also boost levels of good cholesterol. Without regular physical activity, the body slowly loses its strength, stamina and ability to function well. People who are physically active live about 7 years longer than those who are not active and are obese (American Heart Association). Studies have shown that adults who are inactive/minimally active more than 4 hours a day had a 46% increased risk of death from any cause and an 80% increased risk of death from cardiovascular disease!
Also certain medications classically used to help control symptoms of OA are not risk free. The initial algorithm to help maintain symptoms usually follow 3 routes:
1) Nondrug/Non surgical Therapies:
a. Physical therapy/Exercise - strengthen/stabilize muscles around the affected joint
b. Weight Loss – Alleviate pressure from the weight bearing joints (Spine/hip/knees)
2) Medications - used to control inflammation/pain:
a. NSAIDs – Non Steroidal Anti-inflammatory Drugs – one of the most commonly used medications in the world. Advil / Aspirin / Motrin / Aleve / Naproxen / Ibuprofen / Motrin / Diclofenac are all examples of NSAIDs. The issue is they are to be Cautioned/Avoided in individuals with multiple medical issues such as Chronic Kidney Diseae / Congestive Heart Failure / Gastritis or Stomach ulcers / Resistant hypertension.
b. Acetaminophen – commonly recommended when physicians ask patients to avoid NSAIDs. Ex: Tylenol Arthritis – the problem is multiple past studies (and decades of our clinical patient encounters) have shown minimal (if any) anti-inflammatory effectiveness
c. Opioids – Controlled narcotics pain medication that is classified as an unfortunate epidemic in the USA. These medications bind to opioid receptors in the brain/spinal cord and blunt to pain signals. The issue is they have dangerous side effect profile (can be fatal) and also patients develop tolerance and are in need of larger dosages which can lead to a potential addiction or overdose
3) Surgical Options
a. Joint injection – commonly performed by orthopedic surgeons or rheumatologists – typically are either a corticosteroid injection to suppress inflammation locally or a hyaluronic acid injection to provide some degree of joint cushion. The issue is both are short term solutions that typically lead to recurrent issues
b. Joint Surgery – commonly performed by an orthopedic surgeon. Such as a total hip arthoplasty (THA) or total knee arthroplasty (TKA) or spinal laminectomy and/or fusion procedure. The issue is these are invasive surgeries that carry risk of anesthesia/cardiac events/infections/blood clots and may be difficult especially in the elderly population
Above is a detailed overview of this complex but sadly common issue that is rising across our country and in our world. As a practicing Nephrologist (Kidney Doctor) - I generally never get consulted to manage osteoarthritis but end up playing a large role in the symptom control of my patients.
The most common reason for a patient to see a Nephrologist is for a diagnosis of chronic kidney disease. Our goal is to help slow the progression of this CKD by optimizing risk factors that historically damage kidneys and attempt to avoid progression to a need for renal replacement therapy (dialysis or kidney transplant). Every Nephrologist I know would immediately ask a patient to stop all NSAIDs such as Advil / Motrin / Alleve / Naproxen / Ibuprofen along with several prescription strength NSAIDs such as Diclofenac / Voltaren / Celebrex / Indomethacin / Meloxicam. The only regular recommended alternative is Tylenol (Acetaminophen) Extra Strength or Arthritis at recommended dosages to control aches/pains/inflammation. The issue: Acetaminophen has weak data on arthritis/inflammation control
More often than not our patients come back to us saying they are not achieving adequate management without NSAIDs. Opioids are almost never the right answer for osteoarthritis related pain management (they do not suppress joint inflammation and have a very unfavorable risk profile). Injections/surgeries are invasive and have their drawbacks especially in patients with more advanced chronic kidney disease. We had to research this field to find a safe and effective alternative for our patients!
After years of research - we created vegetarian custom compound that consist of all natural extracts such as Nigella Sativa / Curcumin / Fenugreek / Ginger. All ingredients are herbal and have been used for generations in holistic medicine. Clinical study data exists for active ingredients showing affecting anti-inflammatory action at extracted dosages along with a very favorable/minimal adverse reaction profile without any known common detriments to kidney function / blood pressure / cardiac function / stomach lining. Initially we would informally list out some of these ingredients for our patients to try via powder at their own discretion. The results were very good but the taste/difficulty mixing was cumbersome for most. Our solution is a tablet format called Organic Arthritis. I sincerely hope our OA (Organic Arthritis) works to help mitigate the symptoms of OA (Osteoarthritis) and improve the quality of life for many! Thank you for sharing your time with me on this blog!

We all know the importance of staying active and exercising. It is advice we have heard many times as we navigate the twists and turns known as life. Often it is easier said than done especially for those with arthropathy and joint pains. However, we must fight the battle and remain as mobile and dynamic as possible. Because data shows that our quality of life, overall health, and even life expectancy itself are greatly impacted by our patterns of activity.

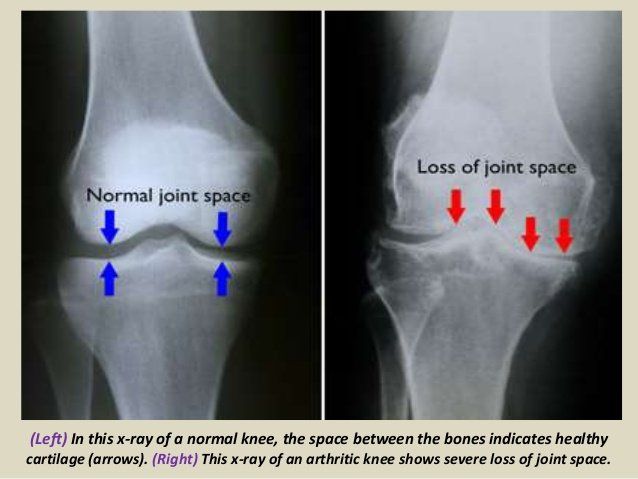
Osteoarthritis is commonly referred to as the “wear and tear” degenerative joint disease. It typically results from the gradual loss of cartilage - the tough connective tissue that is within/between joints. In a way too simple analogy of this complex mechanism - this cartilage serves as essentially a shock absorber preventing direct shear force or “bone on bone” pressure. Once the shock absorber is weakened/gone – trauma will slowly lead to inflammation and erosion of the joint (PAIN!). This leads to a pretty straightforward question - is there a way to repair or at the least slow down the decline of cartilage? Enter Glucosamine - which is an amino sugar and precursor in the synthesis of glycosylated lipids and proteins. It is a natural compound that exists in our cartilage.

Osteoarthritis is one of the most common medical conditions in the world and is commonly referred to as “wear and tear” degenerative joint disease. It typically results from the gradual loss of cartilage within/between joints. This cartilage serves as a type of shock absorber preventing direct shear force and “bone on bone” pressure. Once the shock-absorber is gone it will slowly lead to inflammation and erosion of the joint. US Centers for Disease Control data estimate approx 60 million people with doctor diagnosed arthritis – and remember many people live with joint aches/pain without seeing a physician or getting a formal diagnosis of OA. Sadly the symptoms of OA simply do not stop at the joint. The Arthritis Foundation notes that individuals with OA are almost three times more likely to develop cardiovascular disease (CVD) or heart failure than those without OA. Also, people with osteoarthritis experience as much as 30 percent more falls and have a 20 percent greater risk of fracture than those without OA. These links are especially strong when arthritis is in certain weight bearing/balance joints, such as the knee/back/hip. It makes sense – pain/weakness especially in our stabilizing joints such as knees/hips/spine will limit mobility and lead to risk factors such as weight gain, cardiovascular disease, diabetes coupled with stability issues. These patients would have difficulty following American Heart Association recommendation s that recommend increased physical activity and note that becoming more active can help lower blood pressure and also boost levels of good cholesterol. Without regular physical activity, the body slowly loses its strength, stamina and ability to function well - People who are physically active live about 7 years longer than those who are not active and are obese (American Heart Association). Studies have shown that adults who are inactive/minimally active more than 4 hours a day had a 46% increased risk of death from any cause and an 80% increased risk of death from cardiovascular disease! So now let us focus on some of the clinical presentations of Osteoarthritis (OA). In general there is a marked variability of disease expression. Although most patients present with joint pain and functional limitations, the age of disease onset, sequence of joint involvement, and disease progression vary from person to person. OA ranges from an asymptomatic, incidental finding on clinical or radiologic examination to a progressive disabling disorder eventually culminating in "joint failure" with impaired mobility and quality of life. The primary symptoms of osteoarthritis (OA) are joint pain, stiffness, and motor restriction. Symptoms usually present in just one or a few joints in a middle-aged or older person. Other manifestations in patients with OA include sequelae such as muscle weakness, poor balance, and associated conditions such as fibromyalgia (a disorder characterized by widespread musculoskeletal pain accompanied by fatigue, sleep, memory and mood issues).

Osteoarthritis is oftentimes characterized in simple terms - typically referred to as a “wear and tear” injury to a specific joint. This usually involves the weight bearing joints of the body such as the lower back (lumbar spine), the hips, or the knees but can also include common repetitive use joints such as the fingers/toes and also the ankle (especially if historical trauma/injury is noted). In actuality - osteoarthritis is a complex system with many mediators that can affect degradation of joints/cartilage. There are multiple mechanisms that can help trigger erosive joint disease - including several metabolic triggers. In this excellent review by Wang/Hunter et a l from Osteoarthritis and Cartilage - they have an interesting info graphic highlighting potential metabolic contributors to OA (shared below).

Falls are a major issue especially in our elderly population and falls are the leading cause of injury, both fatal and nonfatal, among older adults in the United States . I can not even count the number of lives that were significantly (and often times permanently) changed after a fall through my decades of practice as a Nephrologist and Internist.

Cultures around the world, originally in eastern philosophy, have utilized mind body movement exercises for generations for various potential mental and physical benefits. These practices have increased in popularity and scope and are now truly global disciplines such as yoga and tai chi . Yoga likely was founded in Indi a and entails discipline in physical, mental, and spiritual realms with originally strong followings in the hindu and buddhist doctrines. It has morphed from being tied to a single country and also bypassed religious connotations. The term "yoga" in the Western world often denotes a modern form of hatha yoga and posture-based physical fitness, stress-relief, and relaxation techniques sometimes accompanied with breathing exercises The focus of yoga in this modern sense is to blend posture based positions/poses to help facilitate exercise for the body and potentially mind. There are many different disciplines/variations of Yoga with significant fluctuations in their physical demands. Many researchers/physicians attempt to quantify the strenuousness of exercises by their energy cost of exercise commonly measured in metabolic equivalent of task (MET). Less than 3 METs counts as light exercise; 3 to 6 METs is moderate; 6 or over is vigorous. American College of Sports Medicine and American Heart Association guidelines count periods of at least 10 minutes of moderate MET level activity towards their recommended daily amounts of exercise. For healthy adults aged 18 to 65, the guidelines recommend moderate exercise for 30 minutes five days a week, or vigorous aerobic exercis e for 20 minutes three days a week. Treated as a form of exercise, a complete yoga session with asanas (body posture) and pranayama (focusing on breath) discipline provides 3.3 ± 1.6 METs which would be classified as an average/moderate workout in strenuousness. There have been several hundred published articles/scientific trials on Yoga and its potential health benefits. Let us focus on some of the data for arthropathy. In one randomized control trial by Deepeshwar et al - Sixty-six individual diagnosed with with knee osteoarthritis (ages between 30 and 75 yo) were randomized into two groups. One group would then participate in yoga for 1 week at a yoga center ( n = 31) and then a control ( n = 35) group who did not participate in any yoga activities. Multiple functional tests were performed on day 1 and then at day 7 - including the Falls Efficacy Scale (FES), Handgrip Strength test (left hand LHGS and right hand RHGS), Timed Up and Go Test (TUG), Sit-to-Stand (STS), and right & left extension and flexion. Results indicated a significant reduction in TUG ( p < 0.001), Right ( p < 0.001), and Left Flexion ( p < 0.001) whereas significant improvements in LHGS ( p < 0.01), and right extension ( p < 0.05) & left extension ( p < 0.001) from baseline was found in the yoga group. This would suggest improved muscular strength, flexibility, and functional mobility in the yoga group. This was a small study that also was completed over a short time frame (1 week) but did show marked functional improvements. Let us look at more data via a large review by Haaz et a l . Researchers combed through peer-reviewed clinical trials (published from 1980-2010) that used yoga as an intervention for arthritis patients and reported quantitative findings. Eleven studies were identified, including four randomized control trials and four non randomized trials. The trials reviewed data is below in the table.

Let us review an interesting study from the Harvard medical system published in the American Journal of Clinical Nutritio n and also Osteoarthritis and Cartilage Journal by Xu et all dealing with the potential impacts of dietary intake patterns and progression of Knee osteoarthritis. There is an age old saying - "You are what you eat" and there has been past data on certain foods/nutrients linked with outcome effects on knee arthritis such as (click the links below for reference articles): Soft drink consumption (potential increased risk of OA progression) Milk consumption (potential decreased risk of OA progression particularly in women) Dietary fat intake (potential increased risk of OA progression) Strawberrie s (potential decreased risk of OA progression particularly in obese adults) Fiber intake (potential decreased risk of OA progression) We also know of many herbs that have varying arthritis control data (some very convincing) and our own Organic Arthritis Herbal Supplement is composed of strong data driven herbs for arthropathy control. There have been past study links between a general Mediterranean diet having a relative lower risk of and improved overall symptom control of knee OA. This study focuses more on overall diet classes and effects on osteoarthritis. This study compares two diet classes based on the Scree test via individual diet questionnaires: Western Diet - composed of high intakes of red and/or processed meats, refined grains, and french fries Prudent Diet - composed of high intakes of vegetables, fruit, fish, whole grains, and legumes

Arthritis is one of the most common medical conditions diagnosed in the United States and world-wide. CDC US data notes there are approximately 60 million individuals battling arthropathy with that estimate rapidly growing to an estimated 78 million (26%) US adults aged 18 years or older projected to have doctor-diagnosed arthritis by 2040 .

Many of us have heard of the medical term INSOMNIA . It refers to a medical condition in which individuals have difficulty falling, staying, or getting back to sleep. There can be short term sleep issues lasting nights or weeks, termed acute insomnia , or long term sleep disturbances ranging months to years, termed chronic insomnia . This can lead to a multitude of general health ramifications. The first question - how much sleep is recommended daily? According to United States Centers for Disease control recommendations - adults should generally have 7 or more hours of sleep nightly to help ensure optimal functional status. This CDC table below helps show National Sleep Foundation and American Academy of Sleep Medicine recommendations: